Treating the body with natural detox after exposure to heavy metals and other poisons

Once you have been diagnosed as having been exposed and or poisoned by heavy metals such as mercury and lead and products such as arsenic and aluminium they need to be successfully removed from the body. This can be done quite easily but then you need to minimize exposure to them so you are not affected once more.
Many life altering changes can occur from acute, a single high dose exposure or ingestion and chronic poisoning a prolonged low dose exposure or ingestion.
Aluminium is one substance that does not occur naturally and it has a high mortality rate of up to 60% on the Indian subcontinent. In the western world aluminium is found in products in our home including foods, cosmetics and saucepans.
Mercury, lead and arsenic are found in the earth’s water, soil and air and is a naturally occurring substance. They are found in ground water and seawater, fresh produce and in the workplace. These substances can all be removed from the body with natural detox methods that include eating foods like garlic and celery.
Treatment
There are chemical treatments available for some and others need some natural methods of avoidance and elimination from our bodies. One method of natural detox is to use reflexology to activate organs and parts of the body to eliminate the toxin. One way that is easy to use at home is to use detox foot pads. These pads are placed on the feet in the evening and left on overnight and then removed in the morning.
This natural detox method works on the reflexology of the foot and will be filled with toxins in the morning. It is amazing how is removed from the body by natural methods.
Methods of natural detox for substances
Mercury
- Chlorella, an aquatic plant, detoxifies connective tissues
- Cilantro detoxifies cells and the brain
- Porphrazyme is a chlorophyll product
- Minerals such as magnesium, sodium, zinc
- Vitamins E, C
Lead
Arsenic
- Celery and cilantro
- Natural detox food pads
Aluminium
- No natural detox is known for toxic doses of aluminium
- For exposure to aluminium around the home you can use garlic, onions and sulphur rich foods
- Use natural detox foot pads at night to eliminate toxins
- Take calcium, magnesium and iron supplements
Get the new detox pads on Amazon here: https://www.amazon.com/BodyPure-Herbal-Remove-Toxins-Natural/dp/B00B4K4WPY/
 These are ventless fireplaces that are made in all types of shapes and sizes. You can have contemporary looking fireplaces with brass or silver linings. Some are made of glass or stainless steel. They are portable to any room and they shut off instantly.
These are ventless fireplaces that are made in all types of shapes and sizes. You can have contemporary looking fireplaces with brass or silver linings. Some are made of glass or stainless steel. They are portable to any room and they shut off instantly.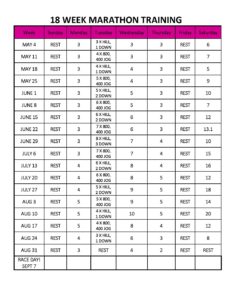
 half marathon training itself. Your physical body needs to time to recover after a training run to prevent injuries as well as aid you create up fitness. Half marathon training timetables have rest days included at normal and also essential times to make sure there is no shed out.
half marathon training itself. Your physical body needs to time to recover after a training run to prevent injuries as well as aid you create up fitness. Half marathon training timetables have rest days included at normal and also essential times to make sure there is no shed out.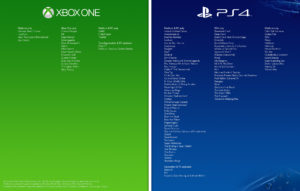 Sometimes, a player feels the urge to turn particular aspects of the game in his/her favor or according to his/her taste. It may be that some part of the game is a bit as well generically hard to conquer as well as is discouraging the gamer; in such cases a skilled gamer usually seeks advice from game hacking short articles on the internet. Game hacking is not officially recommended as it could possibly corrupt the game but that does not stop the neighborhood from altering the game resource code to suit their own requirements and needs.
Sometimes, a player feels the urge to turn particular aspects of the game in his/her favor or according to his/her taste. It may be that some part of the game is a bit as well generically hard to conquer as well as is discouraging the gamer; in such cases a skilled gamer usually seeks advice from game hacking short articles on the internet. Game hacking is not officially recommended as it could possibly corrupt the game but that does not stop the neighborhood from altering the game resource code to suit their own requirements and needs. The best life insurance rate isn’t the cheapest or lowest like most people assume. Exactly what is it then? It is the lowest price that supplies you insurance coverage that does not leave your enjoyed ones stranded. It is the least expensive rate that incorporates the appropriate protection and top quality of solution. If any of these elements are left out after that you definitely have something less than the very best. Just how do you guarantee you obtain it?
The best life insurance rate isn’t the cheapest or lowest like most people assume. Exactly what is it then? It is the lowest price that supplies you insurance coverage that does not leave your enjoyed ones stranded. It is the least expensive rate that incorporates the appropriate protection and top quality of solution. If any of these elements are left out after that you definitely have something less than the very best. Just how do you guarantee you obtain it? Initially, see to it you understand the different kinds of life insurance plans. If you have no idea the benefits and drawbacks of each policy you will not understand which best life insurance rates will serve your passion most ideal. If you get this right after that all other points will certainly start falling in place. This is the 1st step considering that it will definitely form how you set about the various other steps in the procedure …
Initially, see to it you understand the different kinds of life insurance plans. If you have no idea the benefits and drawbacks of each policy you will not understand which best life insurance rates will serve your passion most ideal. If you get this right after that all other points will certainly start falling in place. This is the 1st step considering that it will definitely form how you set about the various other steps in the procedure … The birthplace of karate, the home of rich society as well as traditions and splendid design, Okinawa includes a 1000 kilometers long chain of numerous the Ryukyu Islands that can be separated into 3 primary teams: Okinawa Islands, Miyako Islands, and Yaeyama Islands. In spite of the dispute over the U.S. army bases scattered throughout the islands, there is lots to check out and appreciate in this area; its sandy beaches and also gorgeous coral reefs supply a both relaxing and careless trip as well as thrilling daring water sporting activities.
The birthplace of karate, the home of rich society as well as traditions and splendid design, Okinawa includes a 1000 kilometers long chain of numerous the Ryukyu Islands that can be separated into 3 primary teams: Okinawa Islands, Miyako Islands, and Yaeyama Islands. In spite of the dispute over the U.S. army bases scattered throughout the islands, there is lots to check out and appreciate in this area; its sandy beaches and also gorgeous coral reefs supply a both relaxing and careless trip as well as thrilling daring water sporting activities. Your age your gender additionally has a slight determining element right into just how much you pay each month with women paying slightly less. The last determining element right into just how much you pay per month is the car you drive with four door cars being the most inexpensive to insure as well as two door sports cars being one of the most costly.
Your age your gender additionally has a slight determining element right into just how much you pay each month with women paying slightly less. The last determining element right into just how much you pay per month is the car you drive with four door cars being the most inexpensive to insure as well as two door sports cars being one of the most costly. Jet Lag is a typical affect of traveling that millions of business and also informal tourists struggle with each year. Allow’s begin with a quick definition of just what Jet Lag really is. According to Wikipedia Jet lag is a physical problem, which issues of alterations to circadian rhythms. Circadian rhythms are our physical body’s inner time clock. These rhythms are more frequently referred to as our body clock. Now that we have a brief understanding of what Jet Lag is, lets have a look at exactly how we can avoid it.
Jet Lag is a typical affect of traveling that millions of business and also informal tourists struggle with each year. Allow’s begin with a quick definition of just what Jet Lag really is. According to Wikipedia Jet lag is a physical problem, which issues of alterations to circadian rhythms. Circadian rhythms are our physical body’s inner time clock. These rhythms are more frequently referred to as our body clock. Now that we have a brief understanding of what Jet Lag is, lets have a look at exactly how we can avoid it. Second of all, you need to take an excellent lengthy take a look at the environments. If you see something behind-the-scenes, go look at it very closely, compared to seek out, down, right, left and afterwards look behind you so you won’t miss out on anything that looks excellent.One more regulation you must take into consideration is taking a tripod with you. It matters not if you believe you have a stable hand. If it’s windy, it rainfalls or it snows you will certainly be cold, you will mess up.
Second of all, you need to take an excellent lengthy take a look at the environments. If you see something behind-the-scenes, go look at it very closely, compared to seek out, down, right, left and afterwards look behind you so you won’t miss out on anything that looks excellent.One more regulation you must take into consideration is taking a tripod with you. It matters not if you believe you have a stable hand. If it’s windy, it rainfalls or it snows you will certainly be cold, you will mess up.